How the World Gets Sick and Dies
The results of a project to quantify and understand how human illness is changing on a global scale
The results of a project to quantify and understand how human illness is changing on a global scale
The Manhattan Project created the atomic bomb through an unprecedented combination of brainpower and money. Fifty years later, the same model helped the Human Genome Project map our genetic code. The ambition of these projects was matched only by the public hoopla surrounding them. But last month, with little fanfare, public health revealed its own foray into "Big Science": the Global Burden of Disease.
At its most basic level, the Global Burden of Disease addresses three questions: what makes people sick; how sick does it make them; and what causes people to die? To answer these questions, 486 researchers around the world came together to make model of the world's health. The report, published last month in The Lancet, has no explicit policy positions. But, by creating a holistic portrait of health around the world, it creates unrivaled evidence for how health has changed over time and what areas need the most attention. Health policy and funding from the WHO and many other organizations will focus on the areas of need outlined by the Global Burden of Disease.
When the project began twenty-two years ago, Dr. Christopher Murray, a physician and health economist, and Dr. Alan Lopez, an epidemiologist, set out to quantify human illness: Not only how many people died from liver failure but also how it that impacted their health while living. They could not simply compile existing studies that estimated the number of deaths from diseases because the total deaths in these single-disease studies far exceeded the actual number of people who died every year. Also, mortality data neither captured the impact of debilitating, but never fatal, ailments like lower back pain nor distinguished between the deaths of children and the elderly.
Working from government health data and demographic information, interviews and epidemiological research, Murray and Lopez created statistical models that measure absolute health lost -- imagine Nate Silver's FiveThirtyEight for causes of illness rather than political outcomes. In order to accurately show what diseases cause the most harm to total health, they put years of life lost due to premature death and the impact of living with illness or disability in comparable terms using a unit called the disability adjusted life-year (DALY). A DALY equals one year of life lost due to premature death. To quantify living with illness, values are assigned to represent the disability associated with hundreds of conditions. For instance, living with severe schizophrenia causes disability equivalent to three-quarters of a DALY but mild, chronic neck pain only causes one tenth of a DALY per year.
While the Global Burden of Disease for 1990 relied upon a panel of experts to assign the values to illnesses and disabilities, the Global Burden of Disease for 2010 drew on surveys of the public. In Peru, Bangladesh, Indonesia, Tanziania, and the United States, researchers surveyed low- and middle-income people at the household, and across the world, a similar number were surveyed online. A surveyed person would hear descriptions of two conditions -- such as mild alcohol abuse versus an amputated leg -- and pick the more palatable of the two. Researchers then used these preferences to generate the new set of values quantifying lost quality of life from a given illness. Many experts assumed that across cultures and socioeconomic status, people would have drastically different perceptions of the most disabling disabilities or illnesses -- a farmer valuing physical over mental health while more educated people fear intellectual impairment above all else. But, comparisons of the results from the five countries and online surveys found that peoples' attitudes towards a given condition maintained remarkable similarity. Regardless of the population's character, people value their health in the same ways.
In addition to the public opinion survey, the 2010 Global Burden of Disease dwarfs its predecessor in depth and rigor because of technological advancement and an influx of money.
In 2007, the Gates Foundation donated $105 million to the University of Washington -- the largest university gift ever for public health -- to establish the Institute of Health Metrics and Evaluation (IHME) to oversee this project. Murray became IHME's first director and with him came scores of full time researchers for this project. In addition to the increased size of research team, Dr. Ali Mokdad, Professor of Global Health at the University of Washington, explains that in 1990 "it used to take mainframe computers to do what laptops can do now." Modern computers allow much more sophisticated modeling of the complex interactions between risk factors and diseases around the world. The project has grown such that today's server farms still take days to compile all the demographic information, interviews, and historic and government health data.
For countries with limited or inaccurate registration of illness and death, Dr. Mokdad explained that researchers construct models of the nation's health based on any available information and the health of similar countries. Then, they repeatedly evaluate for accuracy by sampling the country's population and adjusting the model. Together, the newest models for Global Burden of Disease generate 615 million data points.
To track changes in health over the past 20 years, the Global Burden of Disease calculated DALYS, deaths, and major health risk factors for the year 2010 and recalculated data from 1990 with current models. While most of the results remain behind a paywall on the Lancet's website, IHME created a series of interactive graphics that visualize the data for comparisons by year, age group, and geographic region:
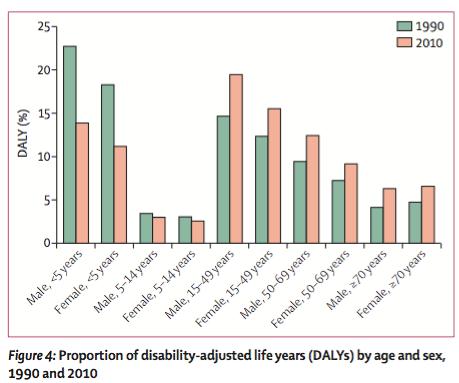
Since 1990, the main source of illness has shifted from infectious diseases (with exception for HIV/AIDS), maternal health problems, and nutritional deficiencies to noncommunicable diseases (NCDs). Even with the HIV pandemic's expansion, the areas targeted by the Millennium Development Goals -- HIV, TB, malaria, maternal and neonatal deaths -- have fallen from nearly 45 percent of DALYs to less than 30 percent. Better sanitation and public health drive this epidemiological transition away from death by pathogens and pregnancy. At the same time, as people live until advanced age, the chronic illnesses that plague the elderly become more common. Taken together, the overall burden of disease has shifted towards more disability in adults.
This trend plays itself out in the top causes of death and DALYs and the top risk factors for poor health. Ischemic heart disease lead all causes in both mortality and DALYs while preventable lower respiratory infections and diarrhea, still both among the top five causes of DALYs, dropped by roughly 50 percent, allowing more children survive into adulthood. High blood pressure and smoking had the greatest risk for poor health. Four of the top ten risk factors directly related to diabetes, the fastest growing major illness with 93 percent more deaths and 69 percent more DALYs than in 1990, as it spreads into the developing world.
Even thought mental health and musculoskeletal problems have to this point received little policy attention, lower back pain and major depression both increased by about 40 percent and landed near the top causes of DALYs. In addition, road injuries, rarely thought of as a public health problem and easily preventable, fell among the top 10 causes of deaths and DALYs around the world.
Overall, the number of DALYs has stayed constant over the twenty years while the world's population has increased by a billion and a half people. This per capita decrease in DALYs at first would seem to demonstrate that people are living healthier lives. However, the amount of disability that people live at any given age has barely changed:
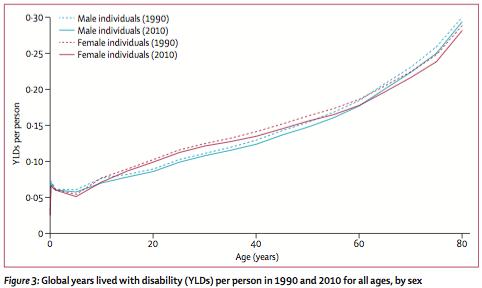
While people live longer than in 1990, they do not live appreciably healthier lives. The decrease in per capita DALYs comes from the approximately 20 percent drop in mortality between 1990 and 2010. According to Dr. Mokdad, especially in wealthier countries, "people are living longer, but they aren't healthier in their extra years." If countries want to improve quality of life for their citizens, they will need to figure out how to control chronic diseases and mitigate disability.
The depth of information provided by the Global Burden of Disease will let policymakers more effectively protect the health of people around the world. By comparing 1990 and 2010, the report will let countries measure the efficacy of their past twenty years of public health policy. Moving forward, understanding what hurts their citizens today will let governments prioritize public health programs and policies that address the areas of most need and will deliver the greatest returns on investment. When overhauling its health system in the early 2000s, Mexico relied upon burden of disease data to prove the areas where it needed to focus most. With the release of the wealth of data from this report, more countries may soon follow suit.
As with all models, the Global Burden of Disease does not perfectly replicate reality. In places where little data is available the results may not accurately represent reality on the ground. And scientists will debate methodological choices in this model -- they already are -- to the benefit of the accuracy of future models. But, even with these flaws, the Global Burden of Disease is valuable beyond its policy results. Just as building the bomb pushed nuclear physics forward and the human genome project transformed the science of computational biology, the herculean task of mapping all of human health drove public health research methods to rigor and complexity previously unseen. The success of this project will be measured not by the accuracy of the numbers it produces but how it informs policy and advances research that improves peoples' lives.
